Photo: Fight For Children
The following article was originally published in the Aspen Institute’s State of Play Washington D.C. report. The report assesses the opportunities and barriers for more children to access sports and physical activity in our nation’s capital.
Since DCPS launched its athletic training program in 1991, student sports participation in the system has tripled while the number of athletic trainers (ATs) has barely budged. The AT shortage was a crucial topic during DCPS teacher contract negotiations in 2024, at which time DCIAA (the district’s public high school athletic league) said it planned to hire a 15th athletic trainer. When DCPS added middle school sports in 2004-05, ATs asked for more staff, but no additions were made, so they became stretched thin even more trying to care for both middle and high school athletes.
“As we added more sports and athletes, that meant more responsibilities for the middle schools, and it became harder and harder to deliver any kind of care,” said Jennifer Rheeling, one of the first ATs in DCPS, who left in October 2023 to serve at KIPP College Preparatory Public Charter School. “A lot of athletic trainers don’t want to work these hours and given the pay. Athletic trainers have compassion fatigue. You can’t be everything to everybody.”
At the time she left DCPS, Rheeling was responsible for athletes at H.D. Woodson High School, Bard High School Early College, Kelly Miller Middle School, Sousa Middle School and about five elementary schools. Through the years, ATs offered proposals to DCPS for three more high school ATs and six more middle school ATs.
“There are dead spots in the system, like charter schools and middle schools,” said Rheeling, a former chair of the National Athletic Trainers’ Association’s secondary school committee. “What scares me is middle school football. It should be either you play tackle football and have an athletic trainer, or you play flag football. During the summer months, there was no one taking care of the middle school kids while we were all at high schools.”
Rheeling said the DCIAA budget also does not allow enough for acquisition of supplies, equipment, maintenance and repair for AT services. Some items that need repair, such as ice machines and golf carts for ATs to travel on while assisting multiple sports teams, fall outside the scope of DGS or needs to be addressed faster than DGS can accommodate.
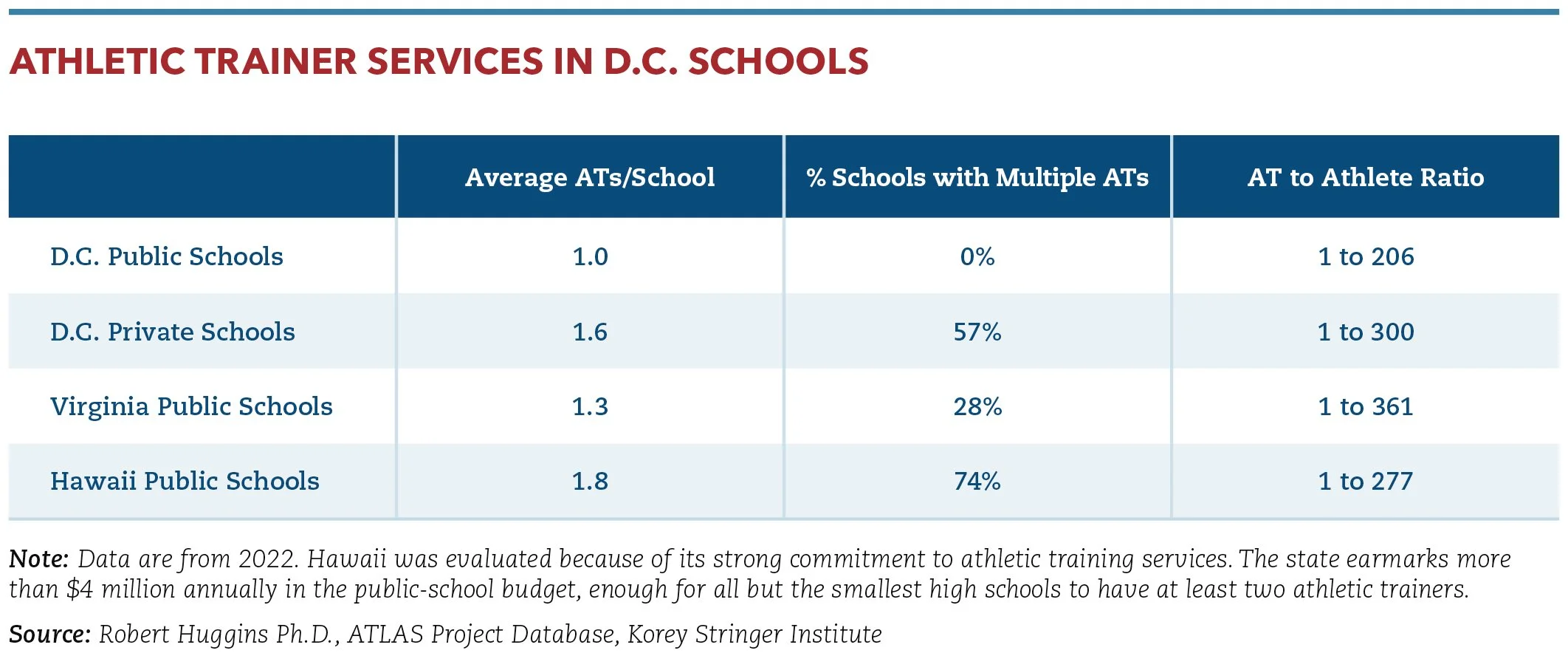
Administrative paperwork and other responsibilities of ATs take too much time away from the delivery of health care. For instance, D.C. public school ATs spend more time on administrative duties (17%) than they do on treatment and rehab, according to research conducted by the ATLAS Project Database through the Korey Stringer Institute.
DCIAA Executive Director Michael Bryant described D.C. as a national leader in athletic training services, noting that other school districts have adopted DCPS’ model.
DCPS partners with George Washington University to provide medical coverage for varsity football games, using licensed medical professionals to help school district ATs evaluate injuries, determine the return-to-play status, and provide referrals for students who may have sustained injuries. “This partnership supplements the work of our ATs in one of our most high-contact sports programs and ensures quality medical coverage for student-athletes at varsity home games throughout the season,” said DCPS Chancellor Dr. Lewis Ferebee.
D.C. is not unique with its AT challenges. Rural and inner-city schools nationally have far less access to ATs than those in the suburbs. Finding athletic trainers to work odd hours and for the amount offered by schools is increasingly challenging. In recent years, the athletic training profession transitioned to require a master’s degree in order to be certified, meaning these students leave college with job opportunities in higher-paying industries than schools, where the sports financial model is backward. Budgets focus first on every aspect related to competition and only then allow for an athletic trainer, if there’s enough money.
Some good news for the District: The D.C. Council passed a bill mandating cardiac emergency response plans in every public, private, public charter, independent and parochial school by the 2025-26 school year. The bill, authored by council member Kenyan R. McDuffie, also requires schools to have at least one automated external defibrillator (AED) for athletic events plus cardiopulmonary resuscitation and AED training for coaches, trainers and school nurses. D.C. joined 13 states that have enacted similar policies.
Solutions
In support of the D.C. high school sports study commissioned by the Office of the Deputy Mayor for Education and released in 2022, Rheeling shared the following ideas on how to improve athletic health care in D.C. schools.
Hire more athletic trainers
Add four 10-month ATs for elementary school sports, six 11-month ATs for middle school sports, and six additional 11-month ATs in select high schools (Jackson-Reed, McKinley Tech, H.D. Woodson, Banneker, Bard and a planned new high school). The three added to existing programs would be event floaters and support larger high school programs where needed. ATs at high schools without football would work a schedule that includes June and July.
Identify separate funding for an athletic training budget
This would ensure availability of supplies, equipment, maintenance and repairs outside the scope of DGS.
Identify and fund an electronic medical record (EMR) system
This electronic system could communicate with other systems and save time for ATs. Such a system could be accessed by hospital systems and accept electronic submission of athlete participation documents. One EMR example is Healthy Roster, which brings forms online, documents injuries and saves time on paperwork.
Create an athletic trainer coordinator position
This dedicated role within DCIAA would oversee the athletic training program.
Add an athletic trainer position to DCSAA
DCSAA, the District’s state high school athletic association, oversees DCIAA as well as private and charter schools. This person’s roles would include:
Oversee policies and procedures related to health and safety in the District
Coordinate training with D.C. emergency medical services
Coordinate medical care at DCSAA events
Oversee the DCSAA Sports Medicine Advisory Committee
Collaborate with other agencies to improve athletic health care throughout the city
Recruit students who want to pursue careers in sports medicine Explore how to fund additional AT jobs by implementing career technical education for sports medicine as an educational offering
Jon Solomon is Community Impact Director of the Aspen Institute’s Project Play initiative. Jon can be reached at jon.solomon@aspeninstitute.org.